Electronic health records (EHRs) have both supporters and detractors. As with most issues, both sides have their share of reason. Which one seems more reasonable may be largely dependent on perspective.
Yet beyond perspectives is the challenge inherent to executing any idea. The concept of an EHR is obviously one geared towards producing a better healthcare future. But getting there can be harder than some imagine.
Consider that one of the main rationales for digitizing healthtech has always been to improve its efficiency, for example. Yet the first implementations of EHR software were actually criticized for making health providers’ work less efficient.
At the root of conflicts like this is perhaps the multiplicity of goals driving EHR technology. To return to the above example, greater efficiency is not the only result sought by those who create, advocate or use EHRs. There is also compliance with state legislation, among others. Sometimes, one goal takes precedence over another.
At any rate, a deeper look into the benefits and disadvantages of adopting current EHR technology would be appropriate for all stakeholders today. We take a look at them below.
- PRO: Future-readiness
- PRO: Higher efficiency
- PRO: Better communication
- PRO: Better data access
- PRO: Better collaboration
- CON: Lost productivity
- CON: Communication barriers
- CON: Lack of interoperability
- CON: Cost concerns
- CON: Security issues
 HITECH is the Health Information Technology for Economic and Clinical Health Act. Enacted in 2009, this law took a carrot-and-stick approach in encouraging US health providers to adopt certified EHR software.
The carrot: incentive disbursements.
The stick: since 2015, providers still not using EHRs have been penalized part of their Medicare payments.
This emphasis on financial penalties and rewards makes EHR usage especially attractive in the US. That said, only cases where certified EHR adoption led to meaningful use of the technology are currently granted incentive payments under the law.
Now what is “meaningful use”? This is a hotly debated topic, but for simplicity’s sake, it signifies use of the software that can be measured in ways set down by the law.
The goal of all meaningful use is to improve healthcare quality. Indeed, improved quality of care should be taken as the foremost benefit ostensibly offered by an EHR. However, as measuring that per se is monumentally difficult, HITECH settles for measuring things that might be termed “indicators” of improvement.
An example of an indicator? How often the EHR is used for e-prescription by a provider.
HITECH is the Health Information Technology for Economic and Clinical Health Act. Enacted in 2009, this law took a carrot-and-stick approach in encouraging US health providers to adopt certified EHR software.
The carrot: incentive disbursements.
The stick: since 2015, providers still not using EHRs have been penalized part of their Medicare payments.
This emphasis on financial penalties and rewards makes EHR usage especially attractive in the US. That said, only cases where certified EHR adoption led to meaningful use of the technology are currently granted incentive payments under the law.
Now what is “meaningful use”? This is a hotly debated topic, but for simplicity’s sake, it signifies use of the software that can be measured in ways set down by the law.
The goal of all meaningful use is to improve healthcare quality. Indeed, improved quality of care should be taken as the foremost benefit ostensibly offered by an EHR. However, as measuring that per se is monumentally difficult, HITECH settles for measuring things that might be termed “indicators” of improvement.
An example of an indicator? How often the EHR is used for e-prescription by a provider.
 Here you see one of the critical issues behind EHR evaluation and regulations. Benchmarks like how often an EHR is used for e-prescription do not necessarily tell you that an EHR is producing an improvement in healthcare. It is simply assumed that doing things like this (e-prescription) more often will lead to such an enhancement.
Put another way, it is assumed that observance of laws like HITECH (regulatory compliance) leads to healthcare improvement.
Regulatory Compliance, the Future, and the Philippines
So are regulations like these coming for the Philippines? Perhaps. Most economic forecasts have the healthtech market growing throughout the coming years. Furthermore, the DOH has already engaged in long-term planning for an e-health and ICT adoption strategy. It may no longer be a question of whether or not we shall get our own version of HITECH, but rather when we shall get it.
Even without regulations, though, there are other considerations. Chief among them for the future of healthcare is this: more and more consumers are expecting digital technology with basic services.
There are those who think that patients do not want digital healthcare services, citing low service usage. Low usage does not actually equate to low interest, however.
A 2014 McKinsey survey across the UK, Singapore, and Germany found that low usage rates were because of poor or inadequate service quality. Over 75% of respondents actually wanted more digital healthcare services, provided those services were of good quality.
Here you see one of the critical issues behind EHR evaluation and regulations. Benchmarks like how often an EHR is used for e-prescription do not necessarily tell you that an EHR is producing an improvement in healthcare. It is simply assumed that doing things like this (e-prescription) more often will lead to such an enhancement.
Put another way, it is assumed that observance of laws like HITECH (regulatory compliance) leads to healthcare improvement.
Regulatory Compliance, the Future, and the Philippines
So are regulations like these coming for the Philippines? Perhaps. Most economic forecasts have the healthtech market growing throughout the coming years. Furthermore, the DOH has already engaged in long-term planning for an e-health and ICT adoption strategy. It may no longer be a question of whether or not we shall get our own version of HITECH, but rather when we shall get it.
Even without regulations, though, there are other considerations. Chief among them for the future of healthcare is this: more and more consumers are expecting digital technology with basic services.
There are those who think that patients do not want digital healthcare services, citing low service usage. Low usage does not actually equate to low interest, however.
A 2014 McKinsey survey across the UK, Singapore, and Germany found that low usage rates were because of poor or inadequate service quality. Over 75% of respondents actually wanted more digital healthcare services, provided those services were of good quality.
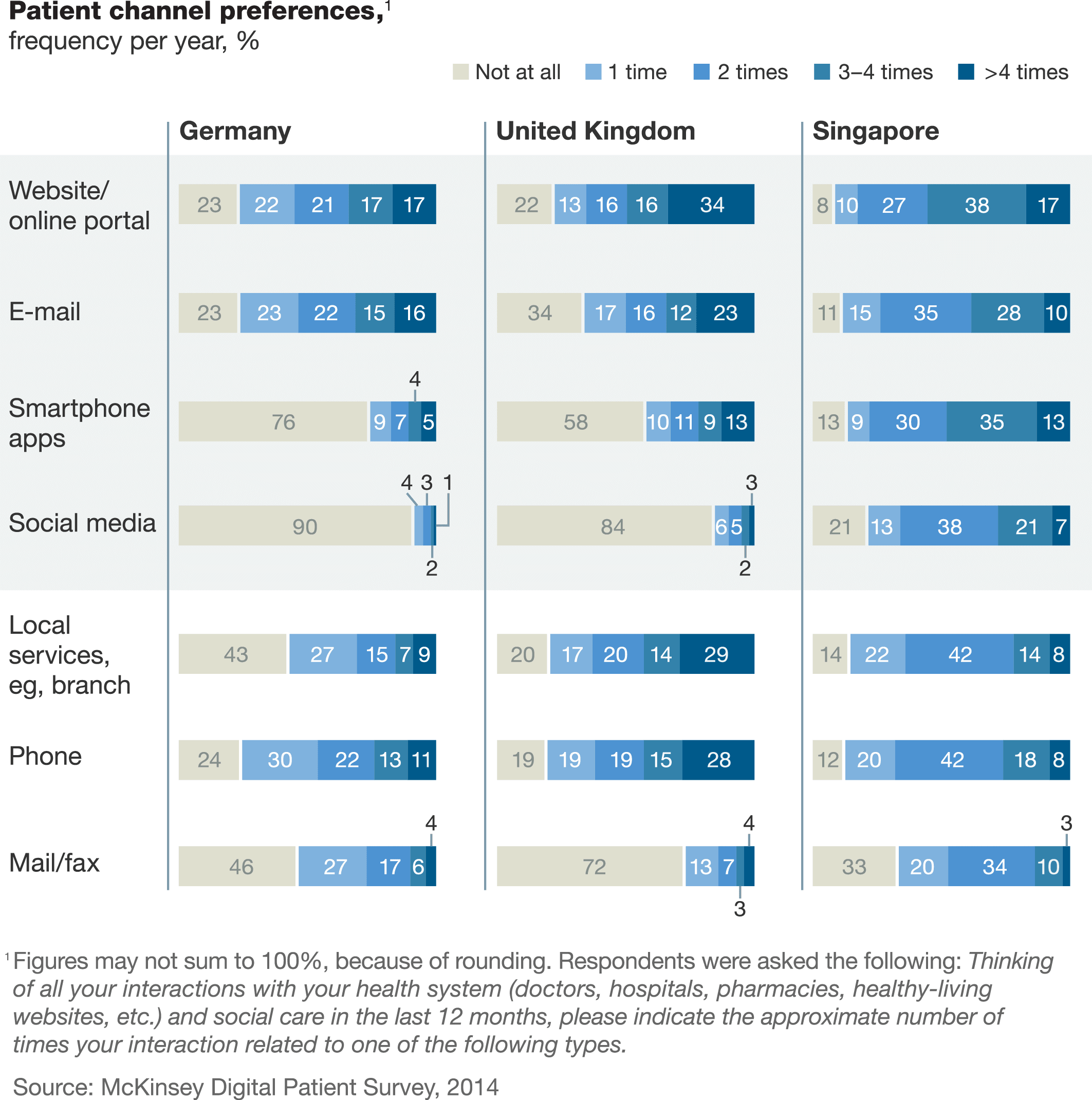
Even with complaints of digital service inadequacy, many patients were already using such services in 2014.

This is just the data for the German respondents; the Singaporean respondents showed even greater interest in digital services among older patients.
- Staff software literacy
- Effectiveness of EHR integration with normal practice workflow
- EHR design (in terms of user-friendliness for providers)
Several of these factors are affected by progress. For instance, it is not unreasonable to suppose that most people would have better software literacy now compared to last year. This might also explain why studies often show higher EHR satisfaction among younger physicians—who are often more comfortable with current technology—than among older ones.
At the same time, technology itself responds to users. EHR creators invest resources in discovering the needs and nitpicks of their customers as the latter react to existing products. These discoveries get fed into new production lines in turn.
That, along with increasing software literacy, may be part of why ratings for many EHRs seem to improve over time. See the difference in users’ satisfaction ratings for the same EHRs in 2016 vs. 2015 from this survey, for instance:
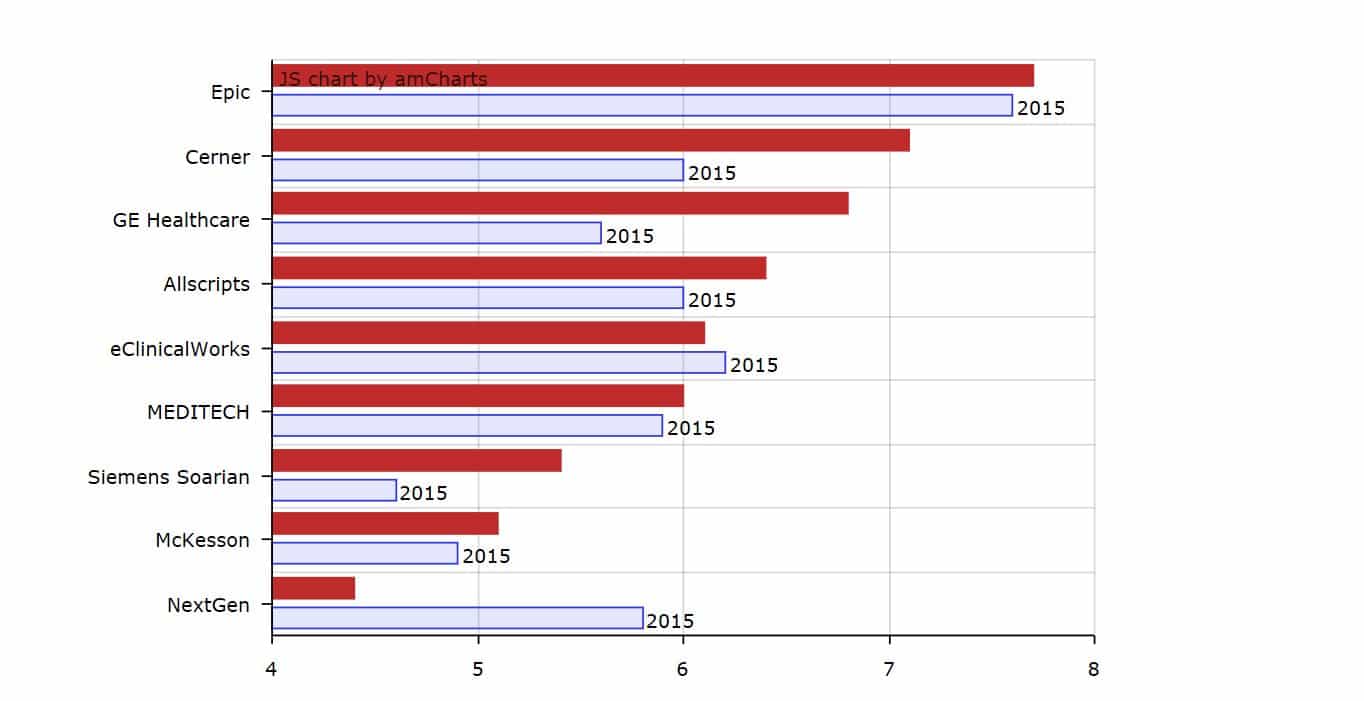
This Health IT News survey shows satisfaction for most EHRs rising from 2015-2016.
This does not mean efficiency as a result of EHR usage is something we only see nowadays. There were already studies as early as 2011 showing efficiency as a result of EHRs. There were even surveys where 79% of providers claimed it to be an outcome.
But how do EHRs lead to efficiency gains, exactly?
Most of the efficiency gains from EHR usage have to do with task automation. Consider some of the tasks involved in file organization alone:
- Physical transportation of patient records to storage
- Sorting medical files
- Manual search of patient records
And so on. Minutes—even hours—of staff labor go into these processes, consuming valuable personnel resources. EHRs can be set up for many of these tasks to be automated.
With EHRs, even the need for physical storage can be reduced if not entirely done away with. Data processing (traditionally a manual task in healthcare) can be automated too: instead of having staff check for possible drug interactions in a patients’ records, physicians can run a check through software instead.
Efficiency gains can translate to financial ones. Greater efficiency from task automation can mean lower personnel costs, for instance. Early studies on EHRs’ benefits even showed efficiency gains making up nearly half of the financial benefits of adoption.
So how should adopters aim for efficiency gains? Perhaps the first thing to work on is evaluating needs and options. Choosing an EHR may be the most important part of the adoption process because different EHRs serve different practices differently.
Many healthcare providers find themselves dissatisfied or replacing the first EHRs they choose because they find them too unwieldy or lacking key features. Yet these are things they could have checked for in advance. Ask questions like these when running your own checks:
- Does the software have the functions you need?
- Does the vendor offer strong, responsive support?
- Are the total costs of adoption within your budget? Remember that some software might actually require an investment in new hardware as well. Some EHRs are not legacy-system-friendly either, so you may end up having to invest in further software upgrades just to get them, e.g. if an EHR requires at least Windows 7 to operate and your computers are still running Windows XP.
- Can the service suffer downtime? SeriousMD works offline, but not all EHRs do. This can be an issue in this country, where we still have unreliable Internet.

EHRs' features are key determinants in selection.
Let us take SeriousMD as an example. Many of our updates have been responses to user requests. Feedback gets funneled to development from multiple sources, from social media (Facebook, Twitter, etc.) to private groups to in-app messaging systems. Some users even meet with us in person and tell us what they think tête-à-tête.
Of course, a filtering system to determine priority requests exists in all companies. Dennis Seymour, one of our co-founders, has spoken about the feedback and filter system used by SeriousMD’s development:
User feedback is one of the most important things when it comes to a product development cycle but of course, we still have to filter out those that won't work. The app is being used by a broad user-base. Different specializations, different operations, different use-cases, different staff numbers and so on.A good example of how filtered feedback has driven development priority would be the SOAP update. A persistent request across various specializations, SOAP made sense for development since it could be tied into further automations across the board. In short, it would render greater efficiency possible for all users, not merely those of a particular specialization.It helps us discover things that we didn't consider during development but it's just as vital to know which one to work on in order to stay on schedule so we can continue to bring value to users.
Take a look at where the EHR you are considering is headed, development-wise. EHR adoption is an investment for long-term gains. Thus, trying to get a sense of each option’s future could help you make up your mind about its potential value to you. You can also list each option’s key features and put lists next to each other for comparison. Contrast often makes choice easier. Take a look at this comparison, for instance. You can look up other EHRs’ feature lists and do further contrast evaluations from there. Take each EHR for a test run too. Most vendors let you request a demo and others offer paid trials (to be refunded if you decide to discontinue the service at the end of the trial period). SeriousMD itself is free and can be accessed without having to submit a request, so you can test drive it at your convenience. Devote time to this process. It would be better to spend several weeks on EHR testing and assessment than to waste thousands of pesos on software you want to replace after a month. Providers should work to find the one that can serve them most effectively… and in so doing, reap true efficiency gains from this technology.
- Remote health monitoring
- Remote appointment scheduling
- Remote prescription
- Remote consultation
EHRs with patient portals allow optimum communication gains of this sort. The patient portal is basically the patient-facing side of the software. Depending on the EHR, patients can see lab results, schedule appointments, access their health records, etc.
There are often concerns about patient portals making things harder for doctors. This is because physicians are afraid that patient messages could swamp them. Yet it might actually be otherwise.

Michigan’s Henry Ford Macomb Hospital had positive experiences with patient portals.
Michigan’s Henry Ford Macomb Hospital implemented an EHR with a patient portal allowing text messages between doctors and patients. The hospital’s program director for Family Medicine, Jeremy Fischer, pointed out that the experience was largely positive.
This was since the text messages actually made it easier for doctors to communicate and for patients to focus on the information. Since patients can also review written/typed communication at leisure, there are fewer chances of them demanding repetition or unnecessary explanations.
Interestingly enough, using EHRs with telehealth facilities may yield even better benefits when managed properly. A study on patients undergoing remote care management (RCM) with data monitoring saw a significant increase in patient engagement. The study also showed that RCM decreased readmissions from 60% to 70% in comparison to the national average.

A cardiologist in a pre-op consultation with a patient and her doctor, who are 400mi away – image from intelFreePress.
In short, using the remote communication, monitoring, and analytical capabilities of current technology could have positive results on both quality of care and provider profitability (through decreased readmission costs).
Ultimately, improved information exchange and provider responsiveness is good for practices. Patients will be less likely to seek other health providers—something they tend to do when they feel they are not taken care of appropriately.
- Referrals across providers can be arranged more easily.
- Providers can send (or share) messages and files directly to (with) each other.
- Easy multipoint file access: say two physicians currently in different locations are consulting on the same patient. Instead of both having to wait for individual copies of the patient’s records being sent or faxed to them, they could access the patient’s files simultaneously on the same EHR.
- CPOE (computerized physician order entry)
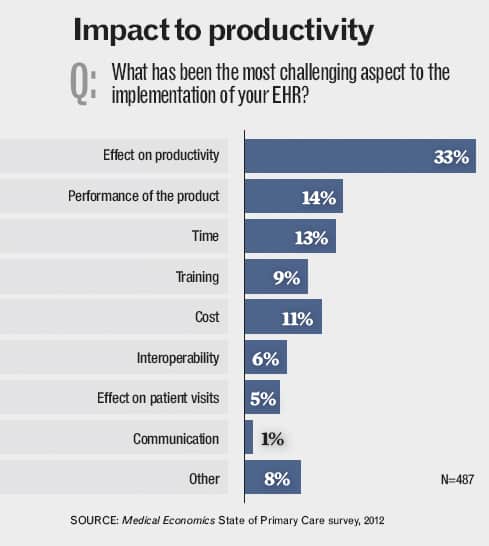
Of the issues adopters face, productivity loss is often considered very important.
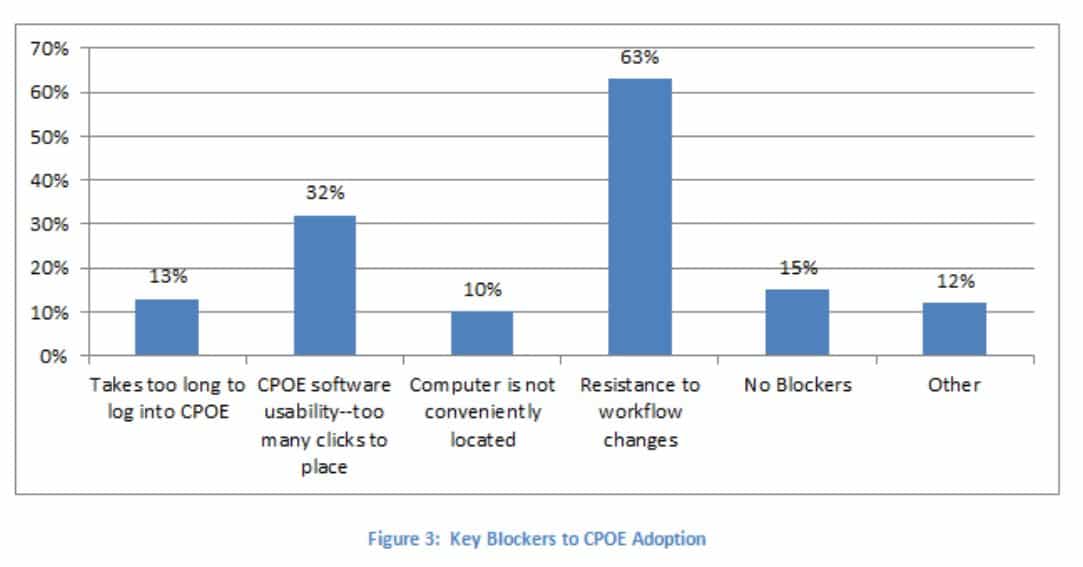
Unwillingness to change can be a powerful barrier.
A triangulated setup could keep patients from feeling excluded.
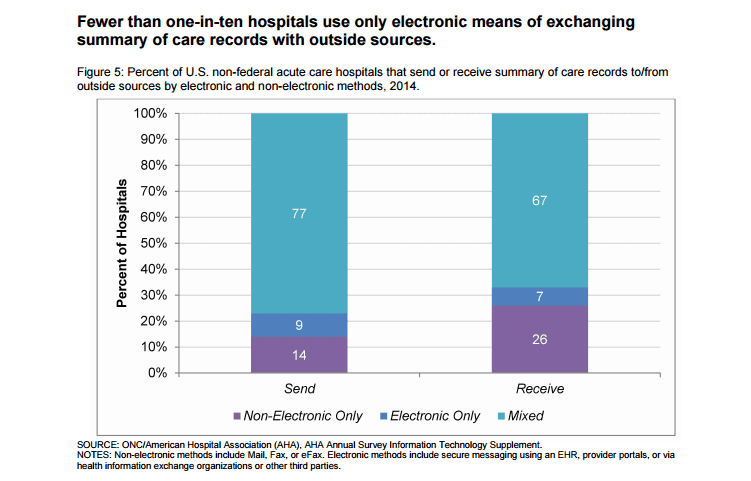
Even as recently as 2014, lack of EHR interoperability was clear in the US.
- Physical hardware – Some EHRs have very specific hardware requirements or minimum specifications. These may require purchase of new components or computing machines.
- Software – Again, this may be required by the EHR because it cannot run on your current operating system.
- Training
- IT support
- Updates
- Security add-ons/support
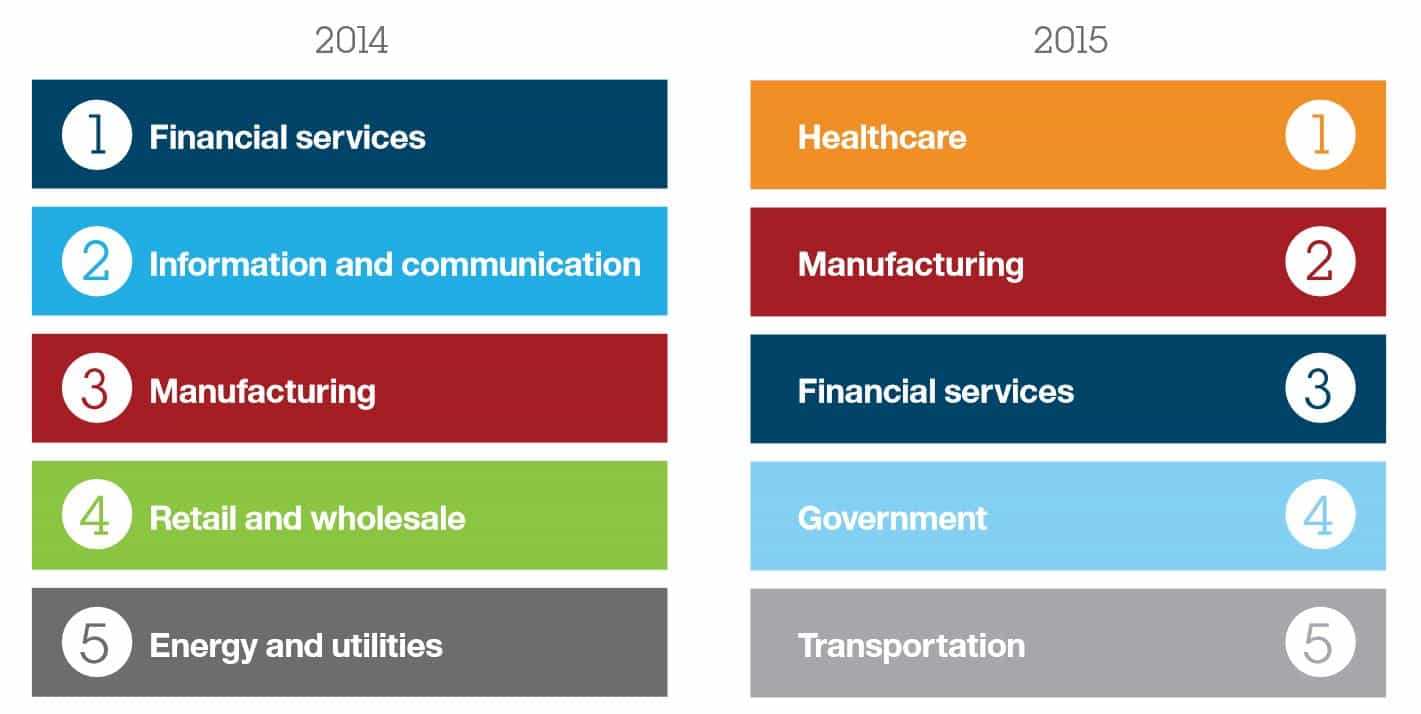
Most attacked industries, from IBM’s 2016 Cyber Security Intelligence Index.
 Are Philippine EHRs Any Better?
Here our lack of an equivalent for HITECH may actually benefit us. Philippine providers are not yet facing the same legal pressures for quick adoption, so users may have better luck here. Local EHR vendors may be able to devote greater attention to security.
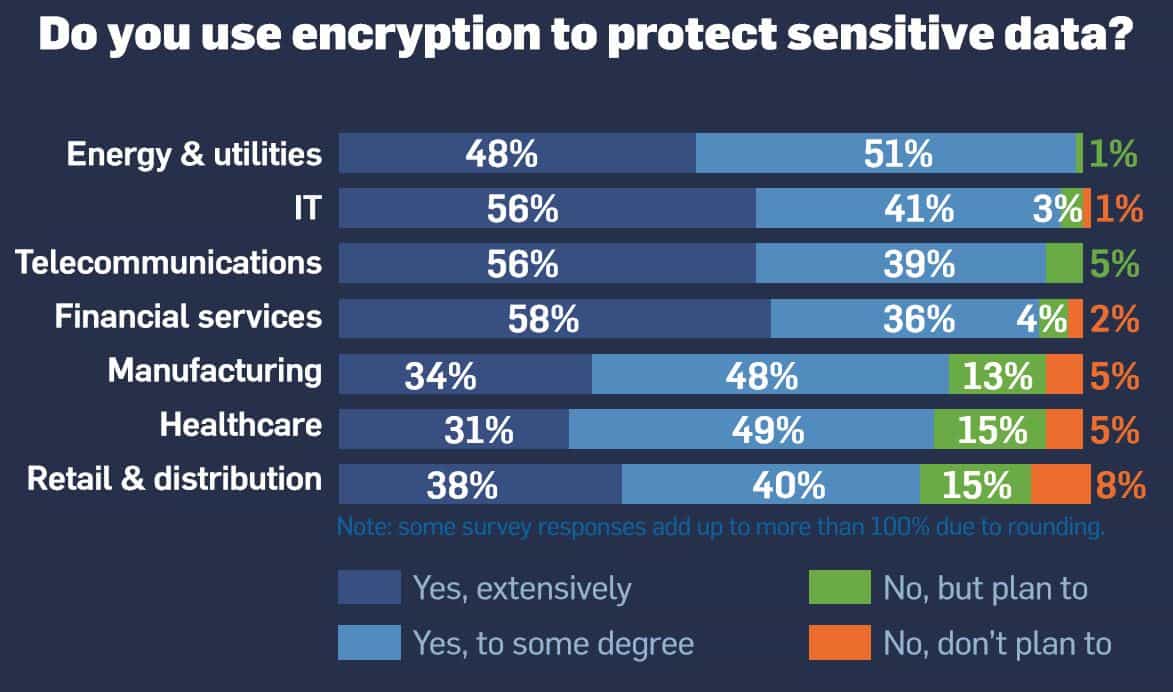
SeriousMD is designed with the latest in encryption technology, for instance. This (strong encryption) is one of the first things one should seek in an EHR’s security. To get an idea of what else you should be seeking, take a look at this page. These should give you an idea of what you need to protect your practice's data.
Are Philippine EHRs Any Better?
Here our lack of an equivalent for HITECH may actually benefit us. Philippine providers are not yet facing the same legal pressures for quick adoption, so users may have better luck here. Local EHR vendors may be able to devote greater attention to security.
SeriousMD is designed with the latest in encryption technology, for instance. This (strong encryption) is one of the first things one should seek in an EHR’s security. To get an idea of what else you should be seeking, take a look at this page. These should give you an idea of what you need to protect your practice's data. Whether it is the pros or the cons that tip the balance may well be dependent on the circumstances of every implementation. What of you? Do you think EHRs right now have more pros or more cons to offer at the moment? Tell us what you think in your comments and in our poll below.
[gravityform id=”12″ title=”true” description=”true”]